A great devotional and prayer by Mike got us started this morning at 6 a.m.: “Dear Lord, today we give thanks for the chance to spread your love to the people of Quezada, to guide our hands as we do your work to heal them of their wounds and their worries. God, we ask that you protect our team, and guide us always as we seek to do your work here, today. In the name of the Father, the Son, and the Holy Spirit. Amen.” And, as Christopher reminded us before breakfast, the challenge today and tomorrow will be keeping our energy up as the temperatures rise. It’s a new group of patients in need, and we want to give them the same care and attention our first 500 received.
After landing at the clinic and opening the doors, I zip over to the “Cucina” for a cup of coffee (even in Quesada, Faith in Practice makes sure we have soy or almond milk). Miguel and his assistants are crucial to this program’s survival. He is the Chef and Head Cook at Casa de Fe (Faith in Practice’s HQ and hospital in Antigua), but he manages all on-site food preparation for the eleven village teams. Miguel makes sure we stay healthy all week with plenty of purified water, coffee, iced tea, snacks, and a fabulous lunch each day. Yesterday it was guisado de pollo, tamales, vegetarian options, as well as sandwiches, piles of fruit, and dessert. We are served something even more exotic today in the blur of work. Lunches are usually a hasty affair timed for low points in the day’s patient flow. It’s a great time to grab a short conversation with fellow staff, or avoid all talk and just go back for seconds. So far, we are all in good health and spirits, and Miguel and his team get much of the thanks and credit for that.
The clinic waiting area is pretty empty around 8:15 as we triage in the first 90 patients, but by 10:30 it’s packed and the clinic traffic is buzzing. Most patients head to a main clinic, sometimes followed by a visit to the lab or sonogram/EKG clinic as needed. But everyone—no matter their age, complaint, or infirmity–inevitably ends up at Farmacia—the Pharmacy. A mysterious room shrouded in secrecy, limited access, and deep tradition (we know what they do, but not how they do it) it is smoothly managed by Bethany who has been on this job for sixteen years. Carmen—a long-time local volunteer–manages stressed out patients, the flow of prescription requests, and the challenging patient education process linked to taking meds (in many cases patients can’t read, so work-arounds have been developed). Carmen reports that Rx fill speed has set a blistering new record under the relentless work-ethic of Aubrie and Heidi, two Ashville-based pharmacists teaming up with Bethany this year. I pray they don’t burn themselves out before Thursday evening.
The massive black boxes lining the pharmacy wall (six in all) contain tens of thousands of pills and liquid suspensions of our formulary–the limited extent of what we have available for patients. It’s a substantial but refined list of meds that hits the sweet spot between patient need, coverage, cost, and restocking challenges. The top five prescriptions this week were vitamins, Tylenol, ibuprophen, eye drops, and stomach meds like Prilosec. For at least the last fifteen years everything pharmacy-related is now purchased, managed, continuously resupplied, and packaged by local Faith in Practice staff. Jessica is with us this week in the village, but back in the Main Office in Antigua she is the Supply Chain Coordinator who makes sure we are set with our promised meds on Monday mornings (no more carrying drugs in by each US team as we used to do in the early 2000s). For long-term supplies of diabetes, hypertension, and birth control meds, government clinics (many more are appearing in small communities, which is a big plus) can be a free or low-cost source for patients. But supply is hit and miss—and patient frustration with that can lower needed medication use. Other sources exist for everything else after our initial patient supply runs out: I counted five pharmacies in towns and in little shopping malls on the way to the clinic this morning. There is great stuff on their shelves, to be sure. The ongoing challenge for people in these impoverished communities, of course, is being able to afford those drugs. And for many/most of our patients, what they receive from us will be all they can get for months because such meds are really priced out of their reach. Pervasive poverty is at the root of the problem. It’s a situation over which we have limited control, but we should all be outraged that most of these patients can’t afford even a meagre regular supply of the most basic analgesics or vitamins. Many of them are fairly beaten down even in their early or late 40s, and these medications (obscenely cheap Stateside) are what are necessary to keep them functioning at work and out of discomfort or pain at home.
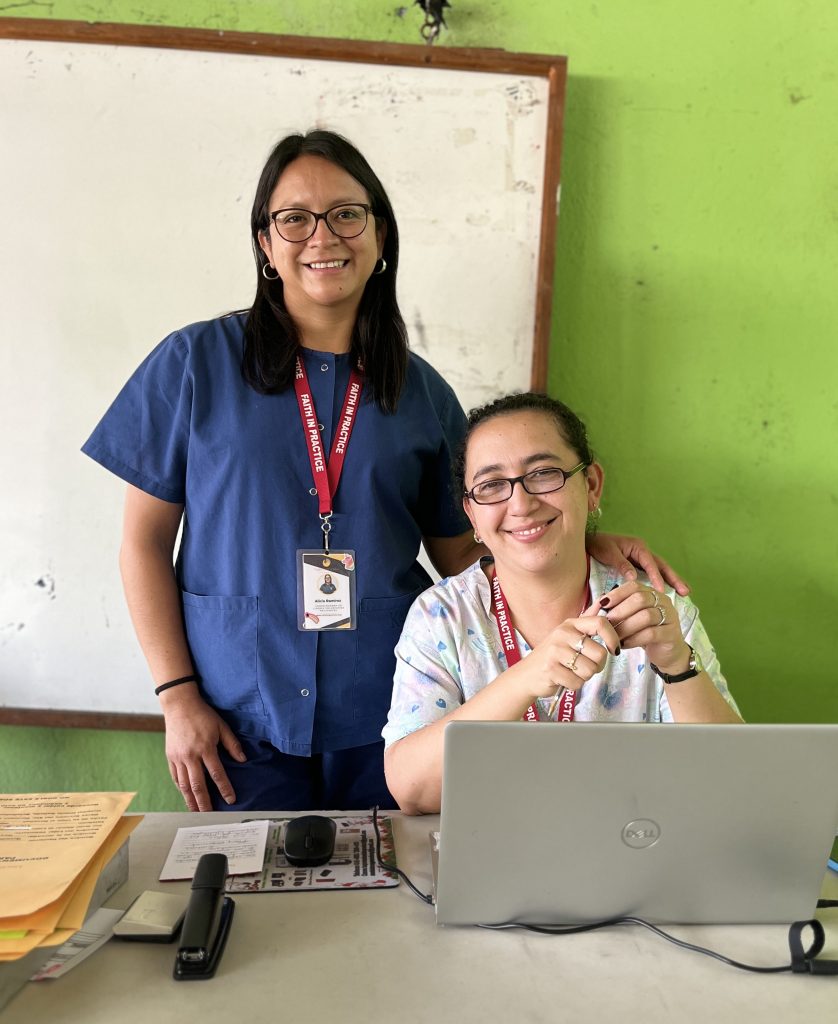
If our week-long village clinic was the last stop in health care provision for our 1000 patients, it would be a tragedy for many, since we can’t adequately address all of their medical challenges. The real gauge of Faith in Practices’s growth and maturity over the past decade is its expanding scope of village clinics and the growing ability of the organization to refer patients to its own surgical units and related care and support facilities. “Referencias”—Referrals—is an important stop for many patients at the end of their visit with us. Buried in official FIP and government forms, courier envelopes, fax and copy machines, and cell phones and laptops, Flora and Alicia manage our major link to next-level-of-care. When we have to tell our patients “there is not much more we can do to help you today,” we can add for some “but we’re going to refer you on for additional follow-up and care.” Sometimes it’s a surgical procedure at Casa de Fe. At other times, its “coordination of care” with other care-givers or facilities. There really is growing hope for serious cases—and Faith in Practice can continue to accompany patients through their ordeal, hopefully to a place of healing and recovery down the road.
During our first two days, Flora and Alicia arranged for 96 referrals—nearly 20% of our patients! Those referrals included gynecological surgery; ear/nose/throat surgery and tonsillectomy; as well as both total hip and total knee replacement surgery. Most of you know a bit about the surgical facilities at Casa de Fe in Antigua. But Faith in Practice now has a Casa and Hospital Hilario Galindo, located in Retalhuleu, about a five-hour drive west of Guatemala City. Faith in Practice surgical teams from the States will start coming in force in April and run through July, taking care of many of the patients that we have sent their way this week. Faith in Practice does such patient referrals more efficiently and at higher quality than any other health care provider in the country.
A tough case presented today in our mobility clinic. A mom and her eleven-year-old-son David, who has cerebral palsy, came in to see if we could assist with a wheelchair. He’s getting to be a big kid, and mom is sinking under the burden of carrying him. Kathy reviewed some therapeutic options for him to increase his strength, back posture, and mobility. We don’t have wheelchairs to provide this week, but a referral for one that will fit his frame means that we can at least give the family some relief in his ongoing care. I always took the growing number of well-trained physical therapy professionals working daily with special needs kids in the schools and community back home for granted. Never again.
Another long but rewarding day of great work. Hope you can reconnect with us again tomorrow.
-Joel Zimbelman
To support this team and their commitment to our patient’s visit: